By Scott Brown MCOptom, BSc(Hons) Optom, Dip OD
Or to re-phrase the question from a more positive angle for Optometrists:
Is Topography Essential for Myopia Control?
The landscape in optometry is changing and it is time for optometrists to really step up and make a difference to the public’s eye sight.
Let’s first talk about glaucoma (POAG). When I first started practicing optometry around 20 years ago there were a small number of elderly patients that suffered functional sight loss due to late diagnosis of glaucoma. In the previous decades IOPs were the main trigger to detect glaucoma and this naturally missed all the normal tension glaucoma patients. Thankfully, I now consider glaucoma likely to cause functional sight loss in only very few patients where even with early detection they do not respond to treatments.
This is thanks to optometry embracing routine glaucoma screening on (probably) all ages of patients. The risk of glaucoma in under patients 64yo 1.43%1. The risk of glaucoma is severe vision loss, generally developing in the over 40s where instrumentation screening is needed to detect vision loss before they are noticed by the patient, and early treatment prevents or limits the disease impact.
To simplify this to my point: glaucoma screening became necessary in routine eye examinations when early detection combined with treatment improved outcome.
I think it would generally now be considered malpractice to not do any glaucoma screening on patients under the age of 64.
Let’s consider another condition, keratoconus.
It develops from childhood and generally before the 40s2. It causes severe vision loss, affects 1.38%3 of the population. Early detection with instrumentation (topography) can lead to corneal cross-linking that stabilises the cornea and reduces the impact on vision.
In practice I see NHS patients for contact lens fitting and see the detrimental affect it has on their lives. In most cases, patients are referred for keratoconus at the point that not only has their prescription has changed significantly over a number of months, but also their VA drops.
Consider the Rx changes over the 10 year period below:
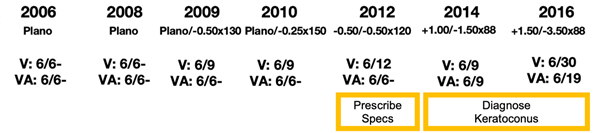
In 2012 there appears to be the start of myopia developing. The improvement in the VA would probably lead us to diagnosing myopia and providing spectacles.
It is not until 2014 that the Rx indicates astigmatism is developing. Corneas reach adult curvatures by 2 years of age4 and in the absence of pathology do not change after 5 years of age6. So a Rx change like this is indicative of keratoconus.
If we now consider the corresponding topography for this patient
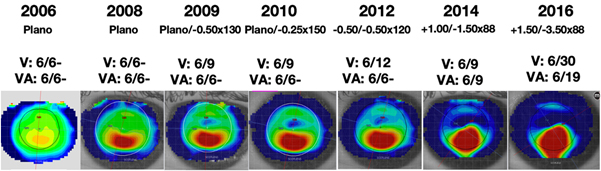
- we can see that in 2006 there is inferior asymmetry
- keratoconus is clearly visible by 2008
- Due to the accuracy of topography this means keratoconus is detectable six years before a Rx change develops
Corneal cross-linking was not available in 2008, but had this been 2021, this patient would have potentially had their vision stabilised at the 2009 level.
Is is negligent, therefore, not to have a topographer?
Topographers are generally considered only necessary for practices that see keratoconus patients or do ortho-k. But this is an attitude that dates back to before corneal cross-linking. Today, neglecting to screen and detect the 1.38% patients that will go on to develop keratoconus, is comparable to neglecting to screen and detect the 1.43% of glaucoma patients.
There is justification for a national screening program and possibly government backing/funding as this could lead to the eradication of sever vision loss due to keratoconus.
However, there is a more immediate issue that should concern us individually as optometrists…
MYOPIA MANAGEMENT
The patient shown above was 11 years old in 2006. In 2012 based on just the Rx change we would probably diagnose myopia and prescribe spectacles.
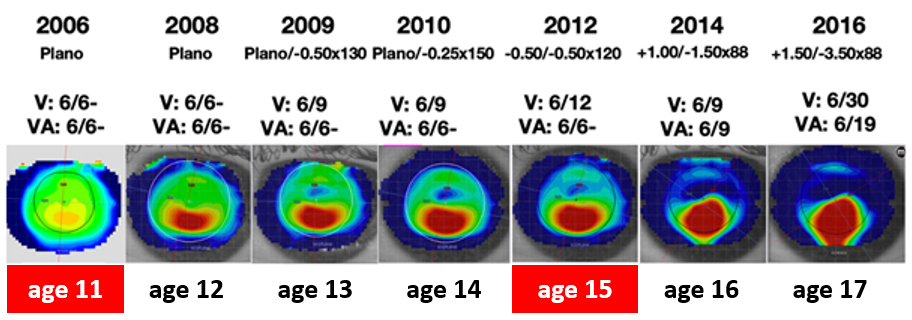
This would be a mis-diagnosis as it is not simple myopia but keratoconus causing a myopic ametropia. Based on this wrong diagnosis the patient is 17yo with progressive myopia, it may be suggested they have a myopia control option. Time would be spent discussing myopia and the options and there would be a significant cost for the patient on the selected option. As topography is necessary for ortho-k this would at least detect the keratoconus at this point if it had been before.
If topography is not performed and a myopia control option is provided, the patient (parents) would no doubt be surprised to be told at follow up that the diagnosis has changed from myopia to keratoconus.
MYOPIA USED TO BE SIMPLE | LESS SO NOWADAYS
Myopia used to be simple. Kids would come in, usually with myopic parents. They would see half way down the chart, we pop a lens in and they get the bottom line. There would be a knowing look from the parent of “It has started then!” and we would provide glasses. Now with specs and soft daily disposable contact lenses that can alter the anatomical development of the eye, optometry needs to not only embrace this, but also step up to providing appropriate examination and care.
MY OPINION
The minimum clinical requirement is that topography should be performed on any patient under 40 with an Rx change. Good clinical practice would be to perform topography on all patients under 40 at routine exams. Jumping on the myopia control bandwagon and selling myopia control spectacles and contact lenses that alter the anatomy of young patient’s eyes beneficially, the same as ortho-k, should be paired with improving ocular examination not only to ensure they are being appropriately provided, but to hopefully see the eradication of keratoconic sight loss.
WATCH: SCOTT DISCUSS THIS TOPIC IN A SHORT 6 MINUTE VIDEO
https://www.youtube.com/watch?v=ZtdwCnItanw
ABOUT THE AUTHOR

Scott Bown MCOptom, BSc(Hons) Optom, Dip OD is the Clinical Director of Scotlens. Scott’s father, Jack Brown, was an Optometrist who was an early pioneer of GP lens designs in the 1970’s launching some of the earliest Ortho-K lenses in the UK. Scott followed in his footsteps as an Optometrist and also an innovative len designer, launching the current stable of custom fit GP lenses, within which was the UK’s first CE GP contact lens and the UK’s first CE Ortho-k lens. Scott has been engaging in Myopia Management with Ortho-K night lenses for over 17 years.
REFERENCES
- Kreft, D., Doblhammer, G., Guthoff, R.F. et al.Prevalence, incidence, and risk factors of primary open-angle glaucoma – a cohort study based on longitudinal data from a German public health insurance. BMC Public Health 19, 851 (2019). https://doi.org/10.1186/s12889-019-6935-6
- Effect of ageing on keratoconic corneas. Millodot M et al. J Optom.2016 Apr-Jun; 9(2): 72–77. doi: 1016/j.optom.2015.05.001
- The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis, Hashemi H et al. Cornea, Volume 39, Number 2, February 2020
- Corneal Curvature and Axial Length Values in Children with Congenital/Infantile Cataract in the First 42 Months of Life. Invest. Ophthalmol. Vis. Sci.. 2008;49(11):4774-4778. doi:10.1167/iovs.07-1564
- Fledelius HC, Stubgaard M. Changes in refraction and corneal curvature during growth and adult life. A cross-sectional study. Acta Ophthalmol (Copenh). 1986 Oct;64(5):487-91. doi: 10.1111/j.1755-3768.1986.tb06959.x. PMID: 3492854.